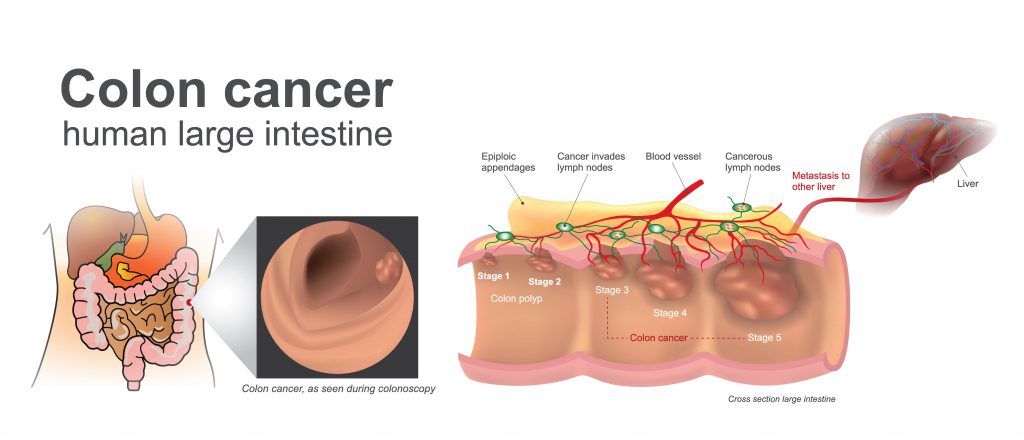
Colorectal cancer is a common cancer worldwide with a low reported incidence in India. About 50,000 new cases of colorectal cancer are reported every year. Nearly 80% of these are detected in advanced cases where offering cure is difficult. The disease typically begins as a non-cancerous polyp which over time, progresses to a frank invasive cancer.
 Over the last few decades, molecular genetic studies have revealed critical mutations underlying the development of colon cancer. These have varied clinical importance ranging from prognostication to targeting them for clinical use in treatment and screening. These have to an extent significantly improved personalised treatment selection for colon cancer.
Over the last few decades, molecular genetic studies have revealed critical mutations underlying the development of colon cancer. These have varied clinical importance ranging from prognostication to targeting them for clinical use in treatment and screening. These have to an extent significantly improved personalised treatment selection for colon cancer.
Here are a few important advancements over the last decade that are likely to impact how we treat colon cancer.
Improved understanding of colon cancer
 Improved understanding of genetic changes in colon cancer has paved the way for a new molecular classification system for colon cancer. The new system enables better prognostication of disease and more personalised treatment selection. This system classifies colon cancer into four molecular subtypes. Colon cancer is no longer a single entity but a heterogeneous group.
Improved understanding of genetic changes in colon cancer has paved the way for a new molecular classification system for colon cancer. The new system enables better prognostication of disease and more personalised treatment selection. This system classifies colon cancer into four molecular subtypes. Colon cancer is no longer a single entity but a heterogeneous group.
Stratifying patients to appropriate risk categories will help treatment planning based on individual risk of recurrence. New pathological markers have been identified in this direction. The current gold standard for stratification is a Tumour Node Metastasis (TNM) system.
‘Immunoscore’ is a novel method that utilises the density of T-lymphocytes infiltrating at tumor core and its margin to generate an overall score. The score was found to significantly influence survival.
Researchers found a new system that combines tumour budding, T cell infiltration and their spatial relationship called Tumor Bud-Immuno Spatial Index (TBISI) to be more effective at-risk stratification.
These newer systems need to be further validated in larger studies before translating into routine clinical use thus providing a more precise prognosis with the ultimate goal of improving patient care.
Advances in surgical management
Interest in minimally invasive surgery, that avoids a traditional open procedure, has increased in recent decades. Robotic‐assisted laparoscopic surgery (RALS) was introduced as the latest advance in minimally invasive surgery.
RALS has the potential to provide better clinical outcomes in colorectal cancer surgery, allowing for precise dissection in the narrow spaces under magnified vision. Though research has not shown robust evidence in support of the notion, it is considered to offer benefits in technically demanding subgroups like males and obese.
Advances in adjuvant treatment of colon cancer
Research all around the world has seen important advances in the adjuvant treatment of early and locally advanced cases of colon cancer. The standard of adjuvant treatment in locally advanced colorectal cancers was chemotherapy with a combination of fluoropyrimidine and oxaliplatin drugs for six months.
Considering the risk-benefit ratio of chemotherapy-related complications versus absolute improvement in survival, studies revealed a three-month duration of chemotherapy is equivalent to low-risk patients. This gives oncologists an opportunity to individualise treatment in this group of patients thus reducing chemotherapy-related side effects in a selected group.
Adjuvant chemotherapy was considered for early-stage (Stage II) colon cancers with high-risk features like tumor spread to surrounding structures, perforation of tumour, inadequate surgery. Preliminary studies suggest the loss of expression of a protein called CDX2 on tumour is a high-risk feature and necessitates the addition of chemotherapy to treatment.
Preliminary studies suggest survival benefit with the addition of Aspirin to chemotherapy in a proportion of patients with a mutation in PI3K, a member of EGFR pathway, a chemical signaling pathway that regulates cell multiplication.
Microsatellite unstable tumours (MSI-H) harbour several genetic mutations that result in the enhanced expression on the tumour cell surface of neo-antigens which trigger an immune reaction to destroy tumour cells.
A new class of agents called immune-checkpoint inhibitors (Opdivo, Keytruda) that have shown activity by blocking a checkpoint protein from binding with their partner proteins and thereby preventing the ‘off’ signal from being sent, allowing T-cells to kill cancer cells. These are approved for use in advanced cancer.
Studies are ongoing in evaluating their use in patients following curative surgery. The results of these studies will help personalise the treatment based on tumour characteristics of individual patients. No one size fits for all!
Understanding of metastatic colon cancer
Performing a few tests to identify mutations in advanced disease is a standard practice that directs the oncologist to select appropriate drugs to control the tumour.
These agents called ‘targeted therapy’ is a standard recommended treatment in metastatic colon cancer. Different groups of these drugs including EGFR inhibitors (Erbitux, Vectibix), BRAF inhibitors (Zelboraf), VEGF inhibitors (Avastin, Stivarga).
Research studies have revealed important information that improved our understanding of genetic alterations in advanced colorectal cancer. This results in better planning of effective drug regimen to individual patients according to the genetic makeup of tumour thus enabling a more personalised approach.
EGFR inhibitors are recommended to patients without RAS mutations and are preferred to anti-VEGF agents. It was found that BRAF inhibitors work well in combination with EGFR inhibitors in tumours harboring BRAF mutations.
Immunotherapy with immune checkpoint inhibitors (Opdivo, Keytruda) has shown benefit in improving survival in a selected group of colon cancer patients harbouring a large number of mutations. These drugs facilitate a patient’s immune cells to target and kill cancerous cells by inhibiting check point blocking proteins. These drugs are approved by the US FDA for use in recurrent and metastatic colon cancer patients.
Trastuzumab (Herceptin), an anti- Her2neu agent, widely used in breast cancer has also shown activity in chemo-refractory patients especially following the use of anti-EGFR agents.
Newer screening tests for colorectal cancer
It is understood for years that colorectal cancer arises as a continuum of progression from a non-cancerous polyp to an invasive tumour with an incremental accumulation of mutations gradually. Screening can reduce the risk of cancer by detection of precancerous growths or detect them early at a stage when treatment is more effective.
Established screening tests include colonoscopy, sigmoidoscopy, virtual colonoscopy, stool-based fecal occult blood tests. Invasive nature of these tests and hence acceptance of individuals to these are main concerns. New techniques employing the genetic analysis of stool samples and those looking at changes in the gut microbiome are underway.
Epi-procolon is an FDA approved blood test for colorectal cancer screening for patients who refuse recommended methods. It detects methylated Septin 9 DNA from the blood of patients with colon cancer. It is a preliminary test primarily indicated for those apprehensive to undergo recommended tests. As a positive test result does not confirm the existence of cancer, all those with positive results should undergo colonoscopy for further evaluation.