From tobacco consumption to genetics, there are various factors associated with cancer. These may be influenced by lifestyle, environment or occupational changes. One such factor, that is known to be linked with various cancer types, is human papillomavirus.
 What is Human Papillomavirus?
What is Human Papillomavirus?
HPV (human papillomavirus) is a group of more than 200 related viruses that are spread between people with skin-to-skin contact. According to Centers for Disease Control and Prevention (CDC), HPV is the most common sexually-transmitted infection, and nearly all sexually active men or women will be infected with HPV at some points of their lives, and some may get infected repeatedly.
Many HPV type infections do not cause any problems, and usually, clear up within a few months after catching the virus. Typically, about 90% clear within two years.
Sexually-transmitted HPVs fall into two categories:
Low-risk HPVs – Usually cause no diseases, but a few low-risk HPV types can lead to warts on or near the genitals, mouth, anus or throat.
High-risk HPVs – These HPV types usually persist and can cause various types of cancers, including the cancer of the cervix. There are about 14 high-risk HPV types, of which HPV16 and HPV18 are responsible for most cancers. These two types (16 and 18) cause 70% of cervical cancers and pre-cancerous lesions in the cervix.
HPV has been linked to various types of cancers that include that of the cervix, vulva, vagina, penis, throat and the anus.
Who is more prone to HPV infections that can lead to cervical cancer?
As stated above, HPV infections are common and most infections won’t last long as the body’s immune system will be able to fight it. But, in some women, the infections may persist and increase the risk of developing cervical cancer. Some of the risk factors are –
- The oncogenicity or cancer-causing strength of the acquired HPV type
- Immune system status – people whose immune system is compromised, such as those who are taking immunosuppressants, or those living with HIV (human immunodeficiency virus) are more likely to have persistent HPV infections that might progress to cancer or precancerous lesions
- Coinfection with other sexually-transmitted infections, such as that of herpes simplex, chlamydia, and gonorrhoea
- Young age while giving first birth and number of babies born
- Multiple sexual partners
- Poor menstrual hygiene
- Tobacco smoking
How does HPV lead to cervical cancer?
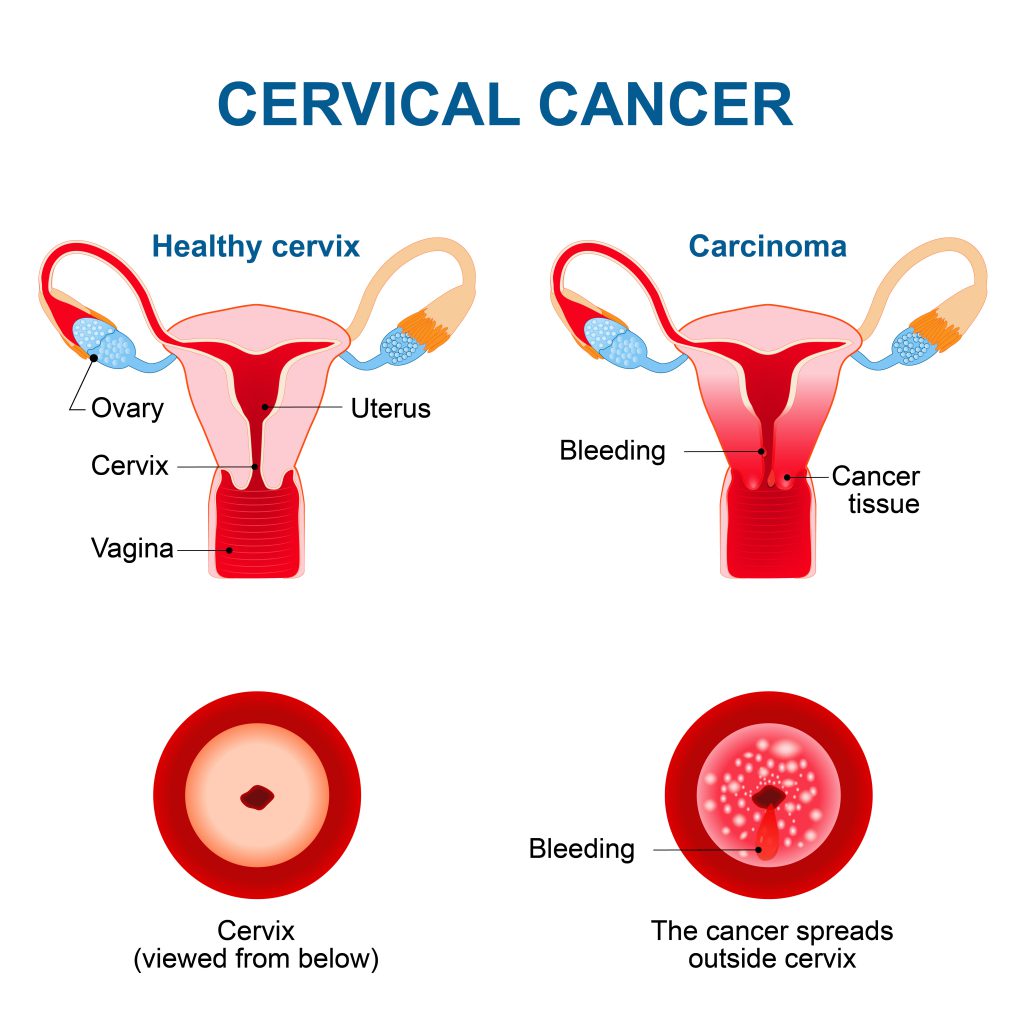
Cervical cancer starts in the cells of the surface layer of cervix, which is the lower part of the uterus that opens to the vagina.
While most of the HPV types are eradicated by the immune system, some types may survive for years. Overtime exposure with the normal cells may start with a viral infection, and eventually, they may develop precancerous changes. This pre-condition is known as cervical intraepithelial neoplasia which usually goes away over time. But, in some cases, it may progress into invasive cervical cancer.
HPV vaccination
HPV vaccines act against both HPV 16 and 18, which are the types known to cause more than 70% of cervical cancer cases. The two common HPV vaccinations in India are Gardasil (that acts against HPV 16 and 18) and Cervarix (acts against HPV 6, 11, 16 and 18). Notably, HPV 6 and 11 are linked to over 90% of genital warts caused by low-risk HPVs.
These vaccines work at their best if administered before exposure to HPV. Vaccination is hence recommended for girls between 9-14 years when most wouldn’t have started any sexual activity. For more information on the age, dosage, and schedule, you can go through the link below.
For women over the age of 23, HPV vaccination is not usually recommended as these women are most likely already infected with HPV and vaccines won’t work.
Know all about HPV vaccination (schedule and dosage) and prevention of HPV related cancers
Screening and treatment of precancerous lesions of the cervix
Cervical cancer screening involves testing for precancerous and cancerous conditions among women who seem to have no symptoms and are perfectly healthy. As precancerous lesions may take many years to develop, screening can detect these precancerous lesions early and can easily be treated. Screening can also help detect cancer in its early stages that can result in treatment with a high cure potential.
According to WHO recommendations, screening is recommended for every woman above the age of 30 and regularly afterward. For women living with HIV and are sexually active, screening is recommended as soon as they know their HIV status.
These are the three types of screening recommendations:
- HPV testing for high-risk HPV types
- Conventional PAP test, and liquid-based cytology (LBC)
- Visual inspection with acetic acid (VIA)
For the treatment of pre-cancerous lesions, WHO recommends cryotherapy (using a chemical to freeze and kill the abnormal cells in the cervix) and Loop Electrosurgical Excision Procedure (LEEP – using mild electric current through a loop of wire, removing abnormal cells in the cervix). For advanced lesions, further discussions with your treating doctor is recommended.
PAP and HPV tests in detecting cervical cancer
PAP test is the commonly recommended screening test for cervical cancer. PAP tests cannot tell if you have had an HPV infection, but can indicate abnormal changes in the cells of the cervix that could be caused by HPV.
An HPV test may be used along with a PAP test, and is used to look for the HPV types that are most likely to cause cervical cancer. Your doctor may recommend an HPV test if –
- Your PAP test was abnormal, showing atypical squamous cells of undetermined significance (ASCUS)
- You are 30 years and older
Guidelines for early detection of cervical cancer
Here are the screening guidelines from American Cancer Society –
Age group of 21 – 29 years
A PAP test is recommended every three years
Age group of 30 – 65 years
PAP test and HPV test every five years (most recommended) or just a PAP test once in three years
For women over 65 years of age
Testing is not recommended if the previous test results were normal (negative), and no pre-cancers were found in the past 10 years. Recent test results of the evaluation should be within five years.
For women who have had pre-cancer of the cervix
For women who have had pre-cancer and treated, regular testing is recommended for 20 years after the treatment of cervical pre-cancer.
For women who had hysterectomy and had their cervix removed
Testing is not recommended unless surgery was performed to treat cervical precancer or cancer.
For women who have already taken the HPV vaccination, the same guidelines can be followed.
Managing invasive cervical cancer
The first identifiable symptoms of early-stage cervical cancer include –
- Irregular blood spotting (spotting – light vaginal bleeding that happens outside the regular periods) in women of reproductive age
- Post-menopausal bleeding or spotting
- Bleeding after sexual intercourse
- Increased vaginal discharge, sometimes with a foul smell
As the cancer of the cervix advances, the symptoms become more severe and may include
- Persistent pain in the back, leg or the pelvic region
- Loss of weight, appetite and fatigue
- Vaginal discomfort or foul smell discharge
- Swelling of a leg or both lower parts
Other symptoms may accompany as well if the cancer is in its advanced stages and has spread to distant organs.
A histopathological examination is required to diagnose cervical cancer and the doctors will take a small piece of suspicious growth (if any) for examination. The cancer is staged depending on the size of the tumour and the extent to which the cancer has spread. Treatment of cervical cancer depends on the stage and the options which might include surgery, chemotherapy and radiotherapy.
If you, or anyone you know, are diagnosed with cervical cancer and looking for the best treatment advice, our expert team of care managers and oncologists can show you the right way.



