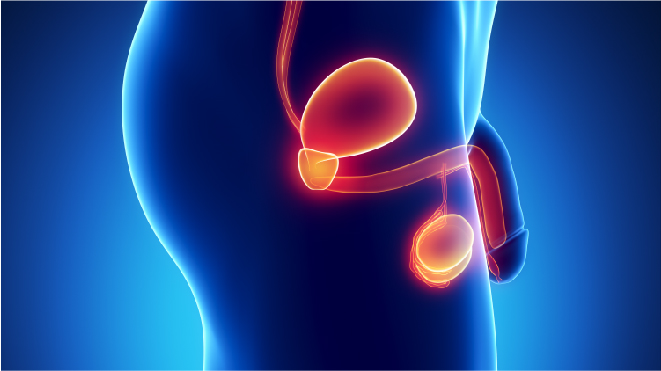
Depending on the tissue or organ where the cancer begins, there are around 200 types of cancers and these are called primary cancers. Some cancers have a high likelihood of spreading from one tissue to another and this is called metastasis. Secondary or metastatic cancers are those that have spread from primary locations, the location where they have first appeared. Testicular cancer is the cancer in the testicles, the male reproductive organ that makes hormones and sperm.
 The testicles:
The testicles:
The testicles or testes (testes is the plural, singular being testis) are male reproductive organs that are slightly smaller than golf balls and held within a sac of skin called scrotum, scrotum hangs under the base of the penis.
Functions:
The testicles have two main functions:
- Production of testosterone, the male hormone in humans
- Production of sperm, the male cells required to fertilize an egg
What are the risk factors?
When the exact causes of a certain type of cancer are not known, certain factors associated with the cancer are identified and are called risk factors. The presence of a risk factor does not imply that the person develops testicular cancer, it only indicates a higher probability. On the other hand, a person may get this cancer even without having any risk factors. The following are the risk factors of testicular cancer:
- Cryptorchidism or undescended testicles is a condition where one or both testicles fail to travel from the abdomen to the scrotum before birth. Men with undescended testicles are more likely to develop testicular cancer than the ones with descended testicles.
- It is observed that people with a history of testicular cancer in the family are more likely to develop testicular cancer than those without.
- Genetic syndromes like the Klinefelter’s syndrome, a condition where the male child is born with an extra chromosome is a known risk factor for testicular cancer.
- Research has shown that men with human immunodeficiency virus (HIV), especially those who have been infected with AIDS have a higher risk of developing testicular cancer.
- The incidence of testicular cancer was higher in the age groups 15 to 35 though it can develop in males of any age.
- Patients with testicular cancer in one testicle are likely to develop this cancer in the other testicle too.
- White men have been noted to be more prone to this cancer type than blacks though the exact cause of this is not known.
Read more about the causes and risk factors here.
What are the symptoms?
Most of the symptoms of testicular cancer show up until the cancer has spread beyond the testicles and the foremost sign includes the enlargement of testicle, hence any lumps or hardness need to be evaluated by a doctor as soon as possible.
Common symptoms:
The common symptoms of this cancer type are:
- Painless lumps on one or both of the testicles which may or may not be accompanied by swelling is a common symptom of testicular cancer. The lumps are initially pea sized though they can grow over time.
- Pain and discomfort in the testicles or the scrotum is another symptom of testicular cancer.
- The feeling of numbness of testicles could indicate testicular cancer.
- Testicular cancer may result in enlargement or shrinking of the testicle.
- Fluid starts to build up in the scrotum which is a reaction to the cancer.
- Swelling of one or both legs or shortness of breath from a blood clot can rarely be a symptom.
Read more about the symptoms here.
Symptoms in advanced stages:
The symptoms in the advanced stages are mostly due to the metastasis of cancer than the original symptoms of testicular cancer and the most common ones are:
- Pain in the lower back
- Shortness of breath
- Bloody sputum or phlegm
- Chest pain
Learn about early detection here.
What are the types of testicular cancer?
Depending on the type of cell the cancer has started in, the type of cancer is determined, the common testicular cancers can be broadly classified into two types- seminoma and non-seminoma.
Seminoma:
This is one of the most curable types of cancer, often observed in men of ages of 30 years to 50 years, there are two main subtypes of seminomas:
- Classical seminomas: It is a slow growing and slow metastasizing form of cancer that accounts almost half of all the germ cell tumours.
- Spermatocytic seminomas: It is a rarer form confined to the testis and has different clinicopathological features when compared to classical seminomas.
Non seminoma:
Non seminomas are tumours in the germ cells but these are more metastasizing than the seminomas as these grow quickly and spread beyond the testicles. There are four main types of non seminomas:
- Teratoma: Tumours in the germ cells of the testicles that cause minimal painless lumps which can be treated by surgery or chemotherapy.
- Yolk sac tumour: Mostly occurring in younger males, the cells lining the yolk sac of the embryo are affected by cancer.
- Choriocarcinoma: Choriocarcinoma is germ cell tumours which metastasizes via hematogenous routes to the lung, liver, brain and other organs.
- Embryonal carcinoma: These tumours are characterized primitive epithelial cells with marked pleomorphism and distinct histologic patterns.
Know more about the types here
How is testicular cancer diagnosed?
Read about the detailed diagnosis here
The following tests are done to confirm the presence of testicular cancer in a patient:
Physical examination:
The testicles are examined for any tenderness, swelling or hardening, light may be projected against the scrotum to see if there are any lumps as they obstruct the light flow.
Scrotal ultrasound:
This is a painless procedure that involves high frequency sound waves to produce the image of the testicles to know if the tumours in the scrotum are benign or malignant.
Tumour marker tests:
A blood sample is taken and is tested for biomarkers that can be elevated in the presence of a particular type of cancer and this test can be performed before and after treatment too, to know the patient’s response to treatment. The tumour markers that help in diagnosing testicular cancer are:
- Alpha-fetoprotein (AFP)
- Beta human chorionic gonadotropin (beta-hCG)
- Lactate dehydrogenase (LDH)
Surgery:
Surgery can also be used as a diagnosis method for testicular cancer as it can help confirm the cancer through biopsy of the cells. This method is not preferred though as there is a risk of the cancer metastasizing and is only used when the other tests are inconclusive.
Imaging tests:
Imaging tests are used for the following main reasons:
- To get knowledge about the spreading of the cancer
- To determine the progress of the patient towards the treatment
- To look for the signs of cancer recurrence post treatment
The imaging tests commonly used in the diagnosis of testicular cancer are:
- Chest x-ray
- CT scan
- MRI
- PET scan
- Bone scan
What are the stages of testicular cancer?
Staging is an essential step for treating the patient as the extent to which the testicular cancer has spread is important to determine the right method of treatment. Cancer types that form tumours are staged using TNM system and the same is used for testicular cancer too.
Staging:
TNM stands for stands for tumour, node and metastasis and the additional parameter for staging testicular cancer is S, the serum level of tumour marker in blood of the patient. In addition to that, a prefix is added to denoted if the stage is clinical or pathological (c or p), for example (cT1, N0, M0).
Stage 0:(pTisN0M0)
In stage 0 of testicular cancer, the cancer has not spread beyond the testicles and the tumours are called carcinomas in situ at this stage.
Stage 1:
The cancer can be any level of T but has not spread to the lymph nodes or to a distant organ, the staging is (anyT, N0, M0).
Stage 2:
The testicular cancer has spread to any number of lymph nodes but not to distant organs and the staging is (anyT,N1-N3, M0).
Stage 3:
The tumour has spread to a distant lymph node or to an organ regardless of the size of the tumour and the staging is (any T, any N, M1).
Learn more about stages here.
How is testicular cancer treated?
The following are the treatment methods of testicular cancer:
Surgery:
Surgery is one of the best methods of treating testicular cancer and can completely eliminate cancer in the early stages and even if the testicular cancer has metastasized, it is essential to remove one or both the testicles if the cancer has affected both. Radical inguinal orchiectomy and retroperitoneal lymph node dissection are the two major surgeries for testicular cancer treatment.
Read more about surgery here.
Chemotherapy:
Chemotherapy uses drugs to kill cancer cells throughout the body and is used if the testicular cancer has metastasized to other organs or if there is a chance of recurrence. It can be used both before the surgery and after as an adjuvant therapy.
Read more about chemotherapy here.
Radiotherapy:
Radiotherapy involves killing cancer cells using high intensity radiation and is also used if the tumours are to be targeted unlike chemotherapy which kills cancer cells in all body parts, however due the risk of radiotherapy to cause infertility, it is used only in case the cancer has spread or can recur.
Read more about radiotherapy here.
Surveillance:
Surveillance refers to the monitoring of the patients under strict medical guidance and is mainly about the healthcare teams having a close watch on the patients so that they do not develop a recurrent or a secondary cancer or show signs that the cancer is spreading.
Stem cell transplantation:
This is rarely used as a method of treatment for testicular cancer as it is not likely that this cancer type spreads too much too fast. It is used to enable high doses of chemotherapy in case the testicular cancer has metastasized to other body organs or if the cancer has recurred. For the treatment of testicular cancer, stem cells of the patient are collected and frozen before chemotherapy and are given back to the patient after.
Read about the other treatment options here.
Fertility issues:
Infertility is defined as the inability to reproduce by natural means, in humans, it means inability to get pregnant or impregnate or carry the pregnancy to its full term. Testicular cancer affects the fertility in males, due to the cancer itself, the pre existing conditions that are risk factors of this cancer or the treatment of testicular or other types of cancers.
Learn more about effects on fertility here.
Orchidectomy:
Orchidectomy is removal of a testicle when it is affected by cancer. In most cases, the cancer is only in one testicle and its removal does not affect the ability to father children. But in some cases, the remaining testicle might not function well and so the person’s fertility may decrease.
Retroperitoneal lymph node dissection:
RPLND is a long and difficult procedure and surgeon will avoid the nerves to prevent nerve damage. But in case of damage or removal of nerves, it can lead to retrograde ejaculation in men. Retrograde ejaculation does not affect the fertility of the person, only their ability to produce children through natural intercourse.
Chemotherapy:
Chemotherapy treatment works by killing the rapidly dividing cells of the body, which usually are cancerous cells. Sperm cells divide quickly too and so become a target for chemotherapy damage. It usually causes temporary infertility that usually goes back to normal some months after chemotherapy, but in some cases the patient might not recover from it.
Radiotherapy:
Radiotherapy involves irradiating the tumour location with high intensity radiation to kill the cancer cells. In testicular cancer, if radiation is used to treat the lymph nodes in the abdomen, there is a small risk that the testicles may receive a small dosage of radiation in spite of using a lead shield to block it.
Follow up:
Post active treatment for testicular cancer also, the patient has to be checking his/her health regularly. This is to check for any signs of recurrence of cancer, manage with the side effects and monitor the overall health.
Managing long term side effects:
In order to cope up with the long term side effects, the patients will have to be constantly monitored by the following tests:
- Heart check-ups
- Lung function
- Hearing function
- Regular electrocardiograms (EKGs)
- Mammography
- Computed tomography (CT) scans
What care has to be taken for testicular cancer:
The follow up plan also includes a proper after care for the patient to follow:
- Regular check-ups with the doctor
- Having small healthy meals 6-8 times a day
- Staying hydrated
- Not working too hard
- Keep skin moisturized
- Take nourishment supplements
- Take anti sickness medication to prevent reduce weakness
- Consult a doctor on any reactions
Read more about the follow up care here.