What is Breast Cancer?
What is Breast Cancer?
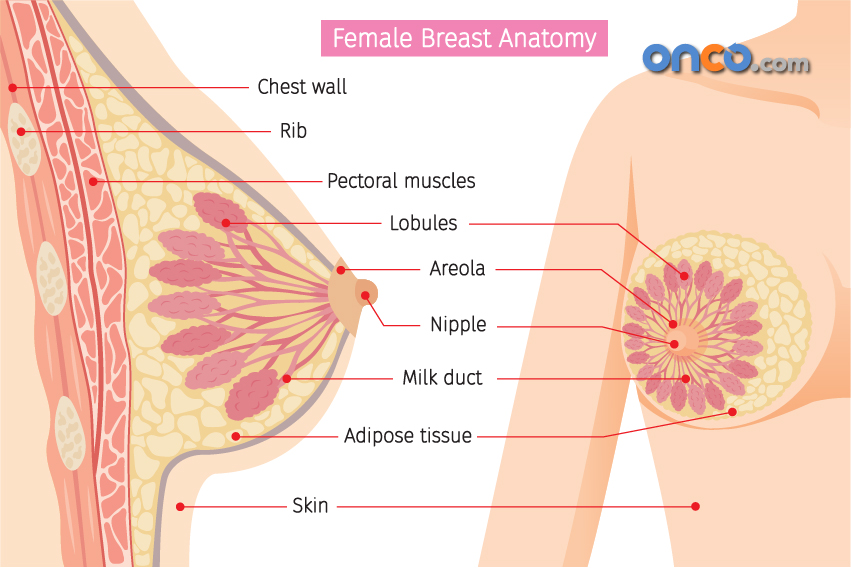
Breast cancer occurs when cells in the breast tissue mutate and divide rapidly. These abnormal cells form a tumour. A tumour can become cancerous when these abnormally growing cells spread to other parts of the breast or other parts of the body. Metastasis refers to the process by which a secondary malignant growth develops at a new site in the body.. Metastasis happens via the bloodstream or the lymphatic system that helps fight infections.
It generally begins in the milk-producing glands (lobules), or in the tube-shaped ducts that carry milk from the lobules to the nipple. Sometimes, it begins taking shape in the fatty and fibrous connective tissue of the breasts.
Both women and men are at risk of developing a tumour in the breast. But it is a hundred times more common in women than in men. It is one of the leading causes of cancer-related deaths in women around the world. But the mortality rates have declined in recent years. Better awareness, regular screening, and advanced treatment options have proved useful.
What are the different types of breast cancer?
Breast cancer can be of different types and sub-types, classified according to the causes, aggressiveness and possible response to treatment. It is important to know the exact type of breast cancer in order for the treatment to be streamlined towards the best possible outcome.
Breast cancer can originate in different parts of the breast area, such as the ducts, the lobules, the connecting tissue between breasts, and in some cases, in the armpit area, where lymph nodes are located.
The treatment for different types of breast cancer depends on the site of origin, the state of invasion (spread) and the dependency of the tumour growth on hormones such as estrogen or progesterone.
Reference guide to understanding the different types of breast cancer:
The type of breast cancer depends on the cells which have been affected. Here are some terms used to describe different types of breast cancer:
- Most breast cancers are carcinomas. Carcinomas are cancers that start in the cells lining the organs or tissues.
- In-situ breast cancers are those that have not spread to the surrounding tissue, which makes them more treatable.
- Invasive breast cancers are cancers that spread from the breast ducts or glands into the breast tissue.
- Metastatic breast cancers are those that have spread to other organs or other parts of the body, such as the lungs, bones, liver, or brain.
- Recurrent breast cancer refers to the return/relapse of breast cancer after a disease-free period, in completely treated patient.
You can read more about the types of breast cancer.
What are the signs and symptoms of breast cancer?
Early detection plays a vital role in the timely treatment of breast cancer. In the early stages, the disease is at small and usually localised and has not spread to nearby organs. In such situations, the right treatment will lead to better outcomes.
Common breast cancer signs and symptoms:
- A painless lump in the breast
- Bloody discharge from the nipples
- Redness of breast in non-lactating women
- Nipple retraction (nipple turning inward)
- Skin irritation or ‘dimpling’
- Scaliness, redness, or thickening of the nipple or thickening of the skin on breasts
- A lump in the underarm area.
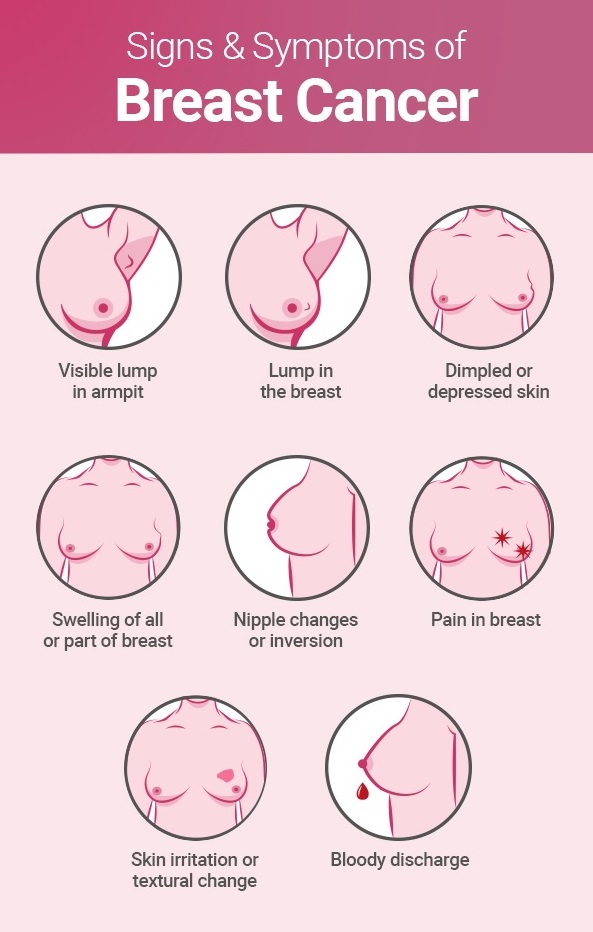
In most patients, a lump in the breast is the first sign of a cancer risk. A lump that is painless, hard, and has uneven edges, has a higher chance of being cancerous. In some cases, however, cancerous lumps may be tender, soft and rounded. Hence, it is essential that a doctor be consulted at the earliest on noticing any unusual changes.
You can read more about the signs and symptoms of breast cancer.
What are the causes of breast cancer?
Changes or mutations in DNA can cause breast cells to develop cancer. DNA is the chemical in our cells that makes up our genes. While breast cancer can be passed on from parents to children, most cases of breast cancer are not inherited in this manner. Lifestyle choices also play a role, including what you eat and how much you exercise. Hormones could also play a role in the growth of breast cancer.
- Most DNA mutations are acquired, which means that the person was not born with this condition but has developed it during his or her lifetime. DNA is present in the genes that tell our cells how to function. When the DNA mutates, the process of how cells divide and die is affected. This causes uncontrolled division of cells, leading to the formation of tumours.
- Proto-oncogenes help cells grow normally. Sometimes, proto-oncogenes mutate to form ‘bad’ genes that are called ‘oncogenes’. Oncogenes cause cells to multiply without control, making more cells than required. This leads to the formation of cancer
- Tumour suppressor genes are normal genes that slow down cell division and control cell death. When tumour suppressor genes don’t work properly then the pace of cell division and cell death is affected. This could again lead to cancer. Examples for tumour suppressor genes are BRCA1 and BRCA2.
You can read about all the factors that play a role in causing breast cancer.
What are the stages of breast cancer?
The stage of the cancer denotes the growth and spread of the cancer. The course of treatment to be followed depends on the stage of cancer. The survival statistics are also based on the stage of cancer.
One of the most common ways of staging cancer is called the TNM system. As the name suggests this system is based on the size of the tumour (T), status of the lymph nodes (N), and the spread or metastasis (M) of the cancer. For each of these factors, a number is assigned between 0 and 4 to show the extent of the cancer. The higher the number the more the effect of cancer on that factor.
The pathological stage of the cancer depends on an examination of the tissue extracted during operation. This is also called the surgical stage. If operating the tumour is not an option then a clinical stage is given to the tumour. This is based on a physical examination, biopsy and imaging tests.
To know more about the different stages of breast cancer and their meaning.
How do I know if I have breast cancer?
Although breast cancer has certain symptoms, many women do not experience any symptoms in the early stages. Cancer discovered in the early stages has a higher chance of a successful prognosis. This is why screening tests play an important role in detecting the cancer in the early stages.
If a woman does not have a family history of breast cancer and has not been exposed to chest radiation therapy, then she is considered to be an average risk of breast cancer. A woman with average risk is recommended a mammogram every year, after the age of 40 years. After the age of 55, this can be reduced to a mammogram once in two years, if no cancer has been detected so far.
It is recommended that all women examine their breasts regularly to spot any signs or symptoms of breast cancer. Women should be familiar with how their breasts look and feel and should be able to spot any changes which need to be reported to a doctor. The most common symptom of breast cancer is a lump in the breast. Self-examination helps in the detection of such lumps while they are still small and can be surgically removed from the breast.
To learn more about the screening tests for breast cancer and how to conduct self-examination of your breasts.
How is breast cancer treated?
Some treatments are called local because they can treat the tumour without affecting the rest of the body. Most types of breast cancer are treated with surgery to remove the tumour. In addition to this, other forms of treatment like radiation therapy may also be used, depending on how advanced the cancer is.
Systemic therapies for breast cancer involve the use of drugs to treat cancerous cells. These drugs are given orally (through the mouth) or intravenously (through the veins). The drugs act on any cancerous cell found anywhere in the body. Chemotherapy, immunotherapy and targeted therapy are examples of systemic therapies.
Although the stage of the cancer is the most important factor is selecting the course of treatment, there are some other factors as well.
- Hormone receptors play a role in deciding the course of treatment, if the cancer is found to be ER-positive or PR-positive.
- The presence of large amounts of HER2 protein in the cells could influence the choice of treatment.
- The overall health of the patient is also considered, along with their age and whether they have attained menopause.
To learn more about the different types of treatment for breast cancer.
What are the survival rates for breast cancer?
Survival rates for different cancer types refer to the percentage of people who are alive and healthy after treatment for the same stage and type of cancer, over a period of time, for example 5 or 10 years. Besides, the available survival rate data cannot serve as an accurate indicator of how long each patient lives with their disease. However, it gives a clearer understanding of the chances of success for a patient’s treatment, depending on the stage and type of diagnosis.
What is a five-year survival rate?
Five-year survival rates for cancer depend on the percentage of people who live for at least 5 years after cancer diagnosis (irrespective of whether they received treatment or not). For instance, if the 5-year survival rate for a particular cancer type is 90%, it means that 90 out of 100 people who had that type of cancer, are still alive after 5 years from their initial diagnosis.
What are relative survival rates for breast cancer?
Relative survival rates are a more accurate method to study and estimate the real effect of cancer on survival. These relative survival rates compare the longevity of the lives of women with breast cancer across the general population. If the five-year relative survival rate for a type of breast cancer is 90%, it means that patients are almost 90% likely to live for five years on an average.
Consequently, it is essential to understand and remember that all five-year relative survival rates are just estimates. The individual prognosis for each patient depends on several factors, the least of which is an average statistic.