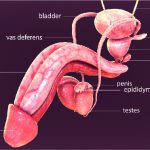
Testicular cancer is the cancer in the testicles, the male reproductive organ that makes hormones and sperm. To learn more about testicular cancer, read here.
What is extragonadal germ cell cancer?
Germ cells are those that develop into reproductive cells of the body and when these cells travel to other parts of the body, they form what are called extragonadal germ cell tumours. These are rare and account for about 1% to 4% of all germ cell tumours. The term ‘extragonadal’ shows that the tumours are outside of the gonads, the reproductive glands, testes in case of males and ovaries in females. These tumours can be benign or malignant, the benign ones also called teratomas account for 80% of the extragonadal germ cell tumours. Teratomas are more common and often very large in size. The malignant EGCs are of two types- nonseminomas and seminomas. Extragonadal germ cell cancer is an aggressive type usually seen in young adults. Read more about the other types of testicular cancers here.
What are the causes and risk factors of EGC:
Extragonadal germ cell tumours are believed to be caused by abnormal migration of germ cells during the development of the foetus. The risk factors of a disease are conditions that are identified to increase the chance of getting that disease, the risk factors of this type of cancer are:
Genetic defects:
Genetic defects in the number of X chromosomes like in Klinefelter syndrome or Turner syndrome in females. Klinefelter is a chromosomal condition where the male is born with an extra X chromosome.
Genetic mutation:
Research has shown some genetic changes in the tumours though only a rare number cases have shown specific genetic mutations.
Family history:
People with a family history of extragonadal germ cell tumours are more likely to develop these when compared to people who do not have it in the family.
Gender:
While benign tumours occur in men and women alike, malignant extragonadal tumours are noted to be nine times more likely in men than in women.
Age:
These tumours have been observed in people of the age group 20 or older.
What are the symptoms of EGC?
Extragonadal tumours can develop anywhere but are usually found in three locations:
- Pineal gland in the brain
- Mediastinum- the area between the lungs
- Retroperitoneum- the back of the abdomen
The symptoms extragonadal tumours are seen as they grow into nearby areas though the exact symptoms depend on where the tumours grow. The symptoms of the disease based on the location of the tumour are as follows:
Brain:
The pineal gland is a small pea shaped endocrine gland that produces melanin, a hormone that regulates sleep patterns. The tumours in the pineal gland are less likely than in the other two locations and the symptoms of this include:
- Increased intracranial pressure due to the tumour can cause nausea, headaches and vomiting
- Depending on the region in the brain the tumour is located in, seizures, movement disorders, visual difficulties and deterioration of intellectual function is possible]
- Early onset of puberty
- Trouble with eye movement
- Diabetes insipidus
- Growth hormone and thyroid hormone deficiencies
Retroperitoneum:
The symptoms can be:
- Abdominal pain or swelling
- Feeling of bloating with nausea or vomiting
- Changes in bowel movements
- Feeling full even on consuming smaller quantities
- Loss of appetite with weight loss
- Fatigue
- Frequent urination with difficulty in urinating
Mediastinum:
The tumours occur in mediastinum 50% to 70% of the time and the symptoms are:
- Difficulty in breathing or swallowing
- Cough
- Weight loss
- Swelling of the face
- Hoarse voice
Diagnosis of extragonadal germ cell cancer:
Get detailed information of the diagnostic tests here.
Physical examination and history:
The general health of the patient is checked along with checking for signs and symptoms of the disease such as lumps or swellings. The patient’s history and habits are noted to know the likelihood of the disease.
Tumour marker tests:
A blood sample is taken and is tested for biomarkers that can be elevated in the presence of cancer. Some of the tumour markers are:
- Alpha fetoprotein (AFP)
- Beta human chorionic gonadotropin (beta-hCP)
- Lactate dehydrogenase (LDH)
Imaging tests
Imaging tests such as CT scan, PET scan, MRI of the chest, abdomen or pelvis can show the presence of extragonadal tumours.
Biopsy:
Biopsy is the removal of the tumour cells to study them under a microscope. Depending on where the extragonadal germ tumour is, an excisional biopsy (removal of a lump of tissue), core biopsy (removal of tissue using a wide needle) or a fine needle aspiration (FNA) biopsy is done.
Treatment of extragonadal germ cell cancer:
The treatment method depending on the location of the tumour, how much it has spread and the type of the tumour too. Some of the treatment options available are:
- Surgery
- Chemotherapy
- Radiotherapy
- Palliative therapy
If the tumour is benign, surgical removal is the best option, but if the location of the tumour is inaccessible or not safe for surgical procedure, non invasive treatment methods like chemotherapy or radiotherapy are used. If the tumour is too large or is likely to spread, debulking surgery is performed followed by chemotherapy and radiotherapy.
Know more about the treatment options of testicular cancer here.