Depending on the symptoms that the patients show, doctors suspect the disease to be testicular cancer. Diagnosing testicular cancer is based on various factors will clear the doctor about the type and stage of cancer, which is helpful for further treatment. Read more about the symptoms of testicular cancer here.

Factors that are considered for determining the diagnosis for the person:
- Type of cancer
- Age
- Medical history
- Signs and symptoms
Know more about testicular cancer here
The following tests are done to diagnose testicular cancer:
Physical examination:
If the patient shows signs of testicular cancer, the doctor might physically examine the testicles which involves feeling the testicles for any swelling, tenderness or hardening. The doctor may also project small light against the scrotum to check if the light passes through it or not. If the lumps in the testicles are solid, their presence obstructs the light, where as the fluid in the scrotum will allow the light to pass through.
Physical examination may also include the checking of abdomen, upper chest, neck, armpits and groin areas for enlarged lymph nodes. Also, legs are examined for swelling which could indicate blood clots in veins of legs, abdomen or the pelvis. The breasts and nipples are checked for growth.
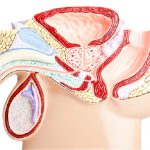
Scrotal ultrasound:
Scrotal ultrasound is a painless procedure which uses high frequency sound waves to produce images of the testicles. These inside images of the testicles help in determining if the disturbances in the testicles are malignant (cancerous) or benign (non-cancerous), along with the position and size of the abnormalities. A fluid-filled lump is non-cancerous where as solid lumps indicate testicular cancer.
Tumour marker tests:
A blood sample is taken and is tested for biomarkers that can be elevated in the presence of a particular type of cancer and this procedure is called tumour marker test. Prior to any treatment, the levels of the serum tumour marker are taken. In testicular cancer diagnosis, they help in determining the stage and type of the cancer. To know more about different types of testicular cancer, go to. However, it is not a necessity that the increased levels of tumour markers must indicate cancer. And it is also possible that testicular cancers do not always raise the serum tumour marker levels.
The following are the tumour markers that help in diagnosing testicular cancer:
Alpha-fetoprotein (AFP):
This tumour marker is not made by seminomas and in most cases, high levels of AFP indicates the presence of nonseminoma.
Beta human chorionic gonadotropin (beta-hCG):
Pure seminoma and non-seminomas, both raise the levels of beta-hCG.
Lactate dehydrogenase (LDH):
This tumour marker is raised by both cancerous and non-cancerous conditions, and is hence rarely used. This is mainly used to determine the dosage of chemotherapy for metastatic nonseminoma.
Placental alkaline phosphatase (PLAP):
This is another tumour marker that is tested for in very rare cases.
Surgery:
Testicular cancers can also be diagnosed using surgical procedures. The general procedure is a biopsy of the tumours, which involves the removal of a small portion of the tumour and examining it under a microscope for cancer cells. This is a very rare option for diagnosing testicular cancer though because it can result in metastasizing the cancer.
Read more about surgery for testicular cancer here
Biopsy is not often used because the results of ultrasound and tumour marker tests are usually conclusive by itself. Based on these results, doctors generally proceed to a surgery to remove the entire tumour. Post removal, it is sent to the lab where it is examined under a microscope for cancer cells.
The diagnosis of testicular cancer is uncertain in a very few cases. In these cases, a biopsy is performed prior removing the testicle. This is done by making a cut above the pubic area and examining the testicle by taking it out the scrotum without cutting the spermatic cord. If cancer is confirmed in the biopsy, the testicle along with the spermatic cord is removed, this is known as orchidectomy. If it’s not cancer, the testicles are returned to the original position.
Imaging tests:
These tests use x-rays, sound waves, magnetic tests or radioactive substances to produce images of the inside of the person’s body. Ultrasound is also a type of imaging test. These tests are done for the following main reasons:
- To get knowledge about the spreading of the cancer
- To determine the progress of the patient towards the treatment
- To look for the signs of cancer recurrence post treatment
Chest x-ray:
X-ray of the chest is taken in order to check if the cancer has spread to the mediastinum, an area in between the lungs.
Computed tomography (CT) scan:
This scan helps in determining the stage of the cancer by examining it’s metastasizing to the other organs.
Magnetic resonance imaging (MRI) scan:
These scans are done to patients in whom the doctors have suspected for the cancer to be spread to the brain or the spinal cord.
Positron emission tomography (PET) scan:
This scan determines small spots of cancer cells in the body, and is also used to check the progress of chemotherapy on the lymph nodes. These scans are more useful for diagnosis of seminomas than nonseminomas.
Bone scan:
Bone scan is taken if the patient has symptoms like bone pain, to check if the cancer has spread to the bone cells.