The first case of COVID-19 was reported in India in January 2020. A year later, India is facing the second wave of this virus.
Most cities in India have seen a sharp spike in the number of cases in April 2021, which has managed to put extreme pressure on both the population and the healthcare system.
Coronaviruses are a large family of viruses that are highly contagious in humans. It can lead to respiratory problems and can escalate very quickly. In some people it is also found to be asymptomatic (without any noticeable symptoms) and could remain unidentified, while continuing to spread to others.
Here we look at what we know about this virus in the second wave, so far, and what it can mean for cancer patients and caregivers in India.
Why are there so many cases of coronavirus in India right now?
The current spike in cases is primarily due to human behaviour. The most basic precautions suggested for containing the spread of the virus have not been adequately followed in many places.
The basic precautions against the spread of this virus include:
- Physical distancing
- Wearing of a fitted face mask
- Hand-washing
COVID-19 has been seen to spread more rapidly in places where all people do not wear masks correctly, and continue to gather in public places for various reasons.
Are cancer patients more likely to get COVID-19?
Having cancer can increase your risk of developing serious illnesses from COVID-19. Other factors that contribute towards this are having a weakened immune system,older age and other pre-existing diseases that affect your respiratory system or your immunity.
Among cancer patients, those with blood cancer may be at higher risk than those with solid tumours.
Will herd immunity protect cancer patients from COVID-19?
Herd immunity is a term used to suggest that if a certain number of people in a community have immunity to a disease then that entire community is protected from an outbreak of that disease.
According to the John Hopkins University, 70% of the community needs to be immune to a disease for it to lead to herd immunity. In the case of COVID-19, most experts agree that unless large scale immunization is successfully completed, herd immunity will not occur.
What can cancer patients do to prevent COVID-19?
The preventive measures for cancer patients and the rest of the population are identical. Here we look at the most basic measures to be taken to protect yourself from this virus:
- Speak to your treating doctor to check if you can safely be vaccinated for COVID-19.
- Follow double masking by using two well-fitted masks to cover your nose and mouth at all times.
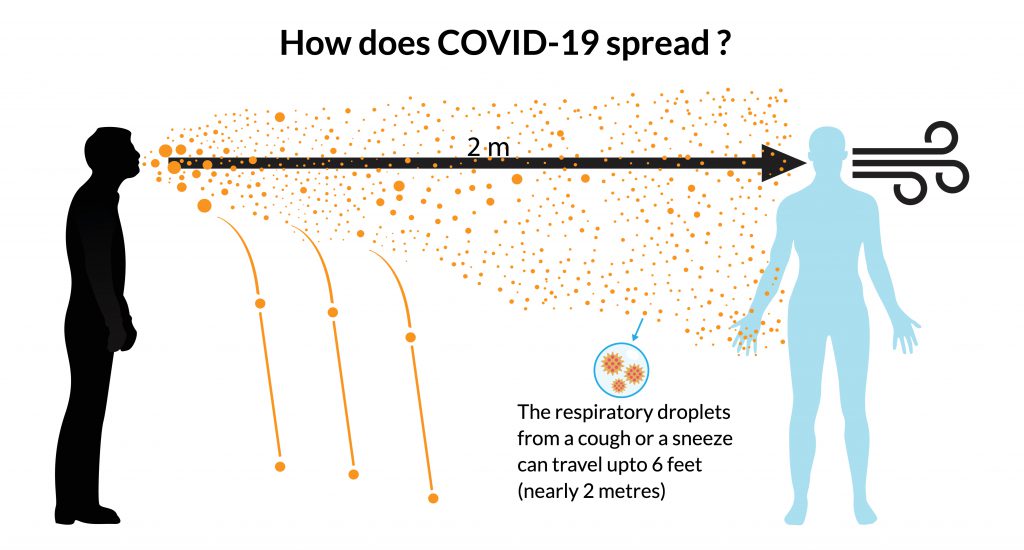
- Stay 6 feet away from anyone that you do not live with.
- Stay home and avoid going outdoors. Do not allow guests into your home.
- Ensure adequate ventilation in your home. You can read more about ventilation here.
- Wash your hands regularly with soap and water. If unable to do this, then use a hand sanitizer frequently.
- Ensure that all surfaces, door knobs and bathroom fixtures are frequently wiped clean with a disinfectant.
- Educate yourself about the symptoms of COVID-19 to watch out for and be alert about these.
What are the symptoms of COVID-19 in the second wave?
In the first wave of this virus, the most commonly reported symptoms were fever, sore throat and a dry cough.
In the second wave, neurological symptoms, gastrointestinal (GI) symptoms, or both might be present. These may occur with or without respiratory symptoms. Other symptoms include muscle weakness, dizziness, tingling in hands and feet, confusion, seizures and stroke.
Gastrointestinal symptoms like nausea, vomiting and abdominal pain have also been reported. The virus has also been detected in stool samples, which is why it is recommended that all toilet fixtures be disinfected regularly.
Extreme weakness and lethargy have been reported as one of the early symptoms of the COVID-19 infection, more so during the second wave.
Several patients have complained of shortness of breath and a fall in oxygen levels, leading to others monitoring their oxygen levels on a regular basis. It’s important to note that shortness of breath without fever or cough could indicate other causes unrelated to COVID-19.
Several patients who have tested positive for the virus have shown no noticeable symptoms. Such asymptomatic persons are still carriers of the virus and could spread it to others if not cautious. Hence, it is necessary to wear a mask even when asymptomatic to protect yourself from contracting the infection and to prevent the spread if you are an asymptomatic carrier.
Management and diagnosis of COVID-19
The approach to initial management of COVID-19 should focus on early recognition of the suspect cases, immediate isolation and disease control measures.
According to the CDC recommendations, specimens from the upper respiratory tract (nasopharyngeal and oropharyngeal swab) are collected to test for the presence of the virus.
Though there is no specific treatment available for COVID-19, the first step in managing it is by ensuring appropriate infection control. The treatment is now done depending on the severity of the disease (mild, moderate or severe disease).
If you feel sick:
- First thing you need to do is to isolate yourself and get tested. It helps contain the spread of infection if one is infected. Consult a physician while at home, and follow what they recommend.
- Ensuring hygiene – clean and disinfect frequently touched objects and surfaces in common areas.
- Monitor Oxygen levels and temperature.
COVID 19 patients with mild disease can be effectively managed with home isolation and treatment. People with moderate disease and severe disease will need hospitalisation. (This is as per clinical need basis; it is recommended that you follow your physician’s advice.)
When should you go to a hospital for COVID-19?
If you have trouble breathing, spo2 < 93% on room air, have persistent fever/ cough, feel constant pain or pressure in your chest or find your face or lips turning blue, you need to get to your nearest COVID-19 treatment centre immediately.



