What is Oral Cancer? The oropharynx is a part of the pharynx (throat). It consists of mainly three subsites which are soft palate, the base of tongue and tonsils. Cancers arising from these areas are categorized under oropharyngeal cancers. These cancers account for nearly 10% of all head and neck cancers. The incidence of oropharyngeal
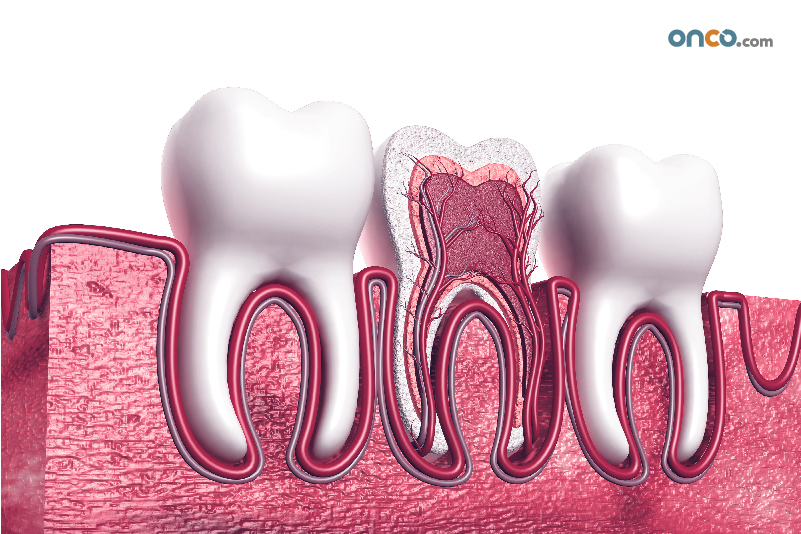
The oral cavity consists of lips, tongue, the floor of the mouth, retromolar trigone, hard palate, alveolar ridge, and buccal mucosa. Cancers of the oral cavity account for approximately one-third of all types of head and neck cancers. Men are twice as likely to get oral cancer as compared to women, and the average age