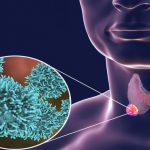
Thyroid cancer is the cancer in the thyroid gland, an endocrine organ which produces hormones that control the speed of metabolism. Read more about thyroid cancer here.
What is radioiodine therapy for thyroid cancer?
This is a type of internal radiation therapy. High doses of a particular form of iodine I-131, which is radioactive is used in the treatment. It is often taken orally in the form of a capsule or liquid. The iodine The iodine circulates in the bloodstream and targets the thyroid cells and thyroid cancer cells. The thyroid cells collect the iodine present in any part of the blood and then, the radioactive iodine kills the thyroid cancer cells. This targeted treatment reduces the risk of harming blood cells in other organs. It is mainly used for treating follicular and papillary thyroid cancers.
When is radioiodine given for thyroid cancer?
This treatment is often given post surgical procedures to remove the residual thyroid cancer that could not be removed by surgeries or for metastasized cancers. Read more about surgery for thyroid cancer here. In few cases, it also given alone as an anticancer treatment for thyroid cancer. The is repeated once in every three months depending on the signs that the recurrent cancer shows.
Preparing for radioactive iodine treatment:
Preparation is the process of making the patients ready for the radioiodine treatment. As a part of this preparation, the patients will be prescribed a man made form of TSH called the recombinant human TSH (rhTSH). It helps the radioiodine treatment by making the thyroid cells able to absorb the radioactive iodine and is generally given for 2 days. Another way of preparing the patients for the treatment is thyroid withdrawal, which involved the termination of any thyroid hormone medication that the patient is taking. The patients who are taking thyroxine (T4) will have to stop the medication for four weeks, while patients who are using liothyronine (T3) will have to stop the medication for two weeks.
The main purpose of thyroid withdrawal is that the radioactive iodine, I-131 functions properly only if the TSH levels in the blood are high, and thyroid withdrawal helps in increasing this value. Some patients are not prescribed thyroid hormone tablets until the surgery and radioactive have finished. The diet of the patient is also very important in preparing him/her for the radioiodine treatment as it helps in reducing the iodine percentage in the body. They are advised to have a low iodine diet. Following are list of restricted and unrestricted foods:
Restricted food:
Patients are not advised to have these foods in high quantity.
- Milk
- Butter
- Cheese
- Dairy products
- Eggs and foods that contain egg
Unrestricted food:
Patients can have the following food in any quantity as they have low iodine:
- Fruits and vegetables
- Bread
- Pasta
- Oils
- Chocolates with minimum 70% cocoa
- Water and soft drinks
- Crisps
- Substitutes for milk
Food that have to avoided:
The following items are to avoided completely because of their high iodine content:
- Seafood
- Green raw vegetables
- Vitamins and minerals supplements
- Fast and junk foods
- Milk chocolate and white chocolate
During radioactive iodine therapy:
This section involves the procedures of how and where the radioactive iodine is given to the patients. The patients who are given the radioactive iodine I-131 are kept alone in a room of the hospital, where they are under constant monitoring for a few days.
Procedure of the treatment:
The radioactive iodine I-131 is taken orally in the form of a drink of capsule. During the treatment, the patient might be experiencing a slight radioactivity, which is why he/she is recommended to stay alone in a single room under constant observation. This monitoring will be done by using a radiation monitor which gives the levels of radioactivity of the patient along with other items that show radioactivity (they have to removed from the room). Only after the radioactivity levels have come down, the patient is allowed to stay come out of the room.
After taking the radioactive iodine, the patient is restricted from eating or drinking anything for sometime, so that the body is given it’s time to absorb the iodine. Post the absorption, he/she can eat normally. The patient is advised to drink plenty of fluids to flush out the radioactive iodine out of the body. During the treatment, the patient’s sweat, urine and the sheets he/she uses are all radioactive.
Protecting others from the radiation:
Since the patients during the treatment are radioactive, they are not encouraged to meet other people, especially pregnant women and children. Other visitors too are not allowed to stay with the patient for more than one hour. The hospital staff, including the doctors and nurses too have limited access to the patients. This is not because the patient is under high risk of radiation, but since the staff gives the treatment to many patients, they have to restrict the dosage that they are exposed to. During the treatment, the patients often advised to take any of their safe interests like books, which do not harm the patients.
Post radioiodine treatment:
As mentioned above, post the treatment, the patient will be radioactive for a few days. They will be under constant monitoring of doctors. Depending on the work out of the patient, the radiation is lost from the body. These measurements are taken from the doctor who evaluate you based on the amount of radiation left in the body. When the radiation has dropped to a safe amount, the patient is allowed to discharge and live with other normal people.
Generally after two to three days of treatment, the patients are asked to get back to their previous medication, especially the thyroxine tablets. These thyroxine tablets are often prescribed for a long run because they restrict the growth and production of the TSH by keeping the thyroid hormones at slightly higher levels.
Precautions to be taken after treatment:
There are certain precautions that every patient has to follow post the treatment because it is radioactive. These precautions change for each individual. Depending upon the dosage of the radiation given, type and stage of thyroid cancer, tolerance and general health of the patient, the doctor shall evaluate and let you know them. Read more about stages of thyroid cancer here.
Following are the most common precautions that all the patients have to follow:
Avoid contact with people:
The patients are asked to stay in a single isolated room with no much access to outsiders because the radioactivity might not be safe for them.
Avoid sharing a bed:
During the treatment, the sheets that the patients use also become radioactive which is why sharing of bed is not healthy and is discouraged.
Sexual contact:
The patients are advised not to have any sexual intercourse during or after a few days of the treatment. Also, women are prescribed a reliable contraception for six months, while men are prescribed for four months. This is because, the eggs and sperms that are produced in this period might have been damaged due to the radiation.
Travelling:
When the patients who are given radioiodine therapy plan to travel by air, they might be stopped at the security because of the radiation alarms. This can happen up to 4 years. So, if the patients wish to travel, they must have a proper medical certificate stating the he/she has been given this treatment.
Side effects of radioiodine for thyroid cancer:
Side effects develop as a result of destruction of the healthy cells in the body during the anticancer treatments.
Common side effects:
The most common side effects of radioiodine therapy in thyroid cancer treatment are as follows:
- Inflammation of salivary glands
- Dry mouth
- Changes in taste
- Nausea
- Swollen it tender neck
Long term side effects:
- Infertility
- Anemia (due to lowered red blood cells)
- Easy bleeding and bruising (due to lowered platelets)
- Prone to infections (due to lowered white blood cell count)
- Lung problems second cancer
- Dry or watery eyes
- Tirednessa
Follow up of radioiodine for thyroid cancer treatment:
The follow up of radioactive iodine is one of the most important part of the treatment. Following are the after care details for the the treatment:
- Have regular appointments with the health care
- Regular diagnostic tests to check for recurrence of cancer and overall health of the patient
- Periodic scanning of the thyroid gland is a compulsion to check for any tumours
- Dynamic risk stratification is done, which is a combination of ultrasound scans and blood tests to check for any
- signs or symptoms of the thyroid cancer. This is generally done 9 months post the treatment.
- Infusion of hormones might be required in case of lowered hormone levels
- Dental care is very important post treatment
Dosage and survival rate:
The initial doses of iodine are slightly higher than the doses that follow, because most of the initial iodine is not absorbed completely and leaves the body in the form of iodine. A few patients will need repetitive doses of the iodine in order to treat recurrent thyroid cancer.
Radioiodine therapy has a high success rate of 90% in treating thyroid cancer. In very few cases, there is a recurrence of the cancer.
Know more about outlook of thyroid cancer here.